America’s hours-long ER wait times for hospital beds are deadly—and experts warn it’s about to get even worse
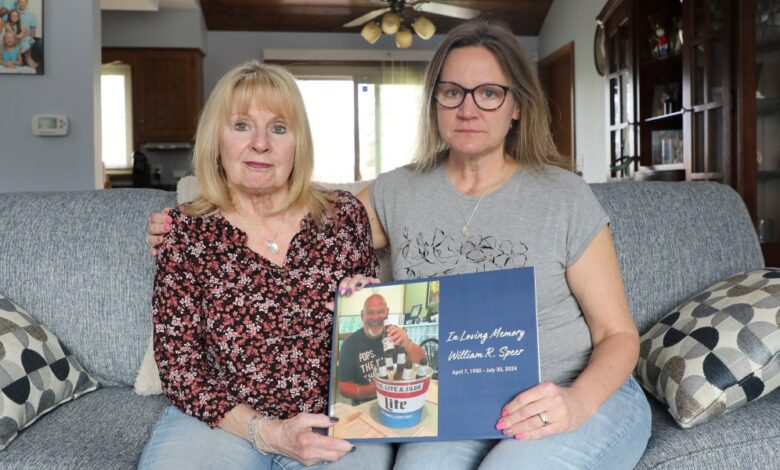

At her mother’s home in Illinois, Trissy Balhan fluctuated her father’s photos, Bill Spere. In one image, smiling in front of a bucket of beer sweat and wears a blue t -shirt reads, “Fixed organic pollutants. Men. Legend. Legend.”
Belhan’s father died last year after he was struggling with himDifference. During a late episode of his life, he became so upset that he tried to get out of a mobile car. She remembers her father – greater than life, fixed and loving – screaming at the top of his lungs.
The psychiatrist for aging recommended him to the emergency room at Edward Hospital in Endifor Health in the Naberfille suburb of Chicago because of its relationship to the behavioral care unit for internal patients. She hoped to help him get a quick referral.
But Speer spent 12 hours in the emergency room – at one point bound by employees – awaiting psychological evaluation. Balhan did not know this after that, but her father’s experience in the hospital is very common, and it has the name: Er Boarding.
One of every six visits toEmergency DepartmentIn the year 2022, which led to the hospital, there was waiting for four hours or more, according to Associated Press andSide effectsData analysis. The analysis showed that fifty percent of patients who had independently of any time of 65 years and over.
Health care experts said that some people who are not in a life -threatening emergency may wait for up to weeks.
ER Boarding is a symptom of health care system conflicts in the United States, including shrinking entry points for patients looking for care outside ERS and hospitals that prioritize the family to the procedures that insurance companies pay more.
Experts also warn that the issue of ascension may get worse asThe number of people is 65 and above in the United States with dementiaIt grows in the coming decades. Hospital bed capacity may not last in the United States. Between 2003 and 2023, the number of hospitals with employees was fixed, even with the emergency department visits by 30 % to 40 % during the same period.
The number of hospital family in the case
For the elderlyWith dementiaDr. Shafi Sidiki, the psychiatrist at Chicago, said Dr. Shafi Sidiki. oneSearch letterIt was published in June 2024 in the Journal of the American Medical Association in more than 200,000 patients and found that long stays can be related to an increase in the risk of dementia who develop delirium – a temporary condition of mental confusion and sometimes hallucinations.
“People need anger (ascending),” said Dr. Vicky Norton, President of the American Academy of Emergency Medicine.
National emergency doctors have pressed for years to continue control. Although she has made some progress, anything has not changed, although fears that it leads to worse results for patients.
Dr. Alison Haddouk, head of the American College of Emergency Doctors, said that this is that ascending to ascending is a failure in the entire health care system that is manifested in ER, and therefore its solution requires a systematic approach.
Argon Venkatish, who is studying emergency medicine at Yale University, said the federal and state political decisions taken about 40 years ago limit the number of hospital beds. He said that people now live for a longer period, which leads to more complex diseases.
In 2003, there were 965,000 hospital hospital beds compared to 913,000 in 2023, according to the American Hospital Association. And another and otherSearch letterIt was published in February, showing that there is 16 % less than the United States employees after birth.
Priority may be given to “scheduled scheduled care” patients who need unavailable procedures, such as caring for cancer or bone surgeries. Haddock said that insurance companies pay more hospitals for these surgeries, so it is unlikely that hospitals will transfer patients to this family – even with the full emergency rooms.
Where can people go?
Emergency medical experts said that although long residence in the emergency department is common, there is no good data that tracks extremists.
Medicare and Medicaid service centers recentlyEndHospitals follow the “mediator” waiting times in their emergency departments. The advisory group, which developed the quality standards of CMS, recommended that the agency try to obtain long long stays. This procedure was recently presented to the CMS, which can choose it.
Patient families are concerned that the long emergency room may make things worse for their loved ones, forcing some to search for limited alternatives to operate for support and care.
Nancy Freija lives in Kangaki, Illinois, with her husband Michael Ryman, who suffers from dementia.
Last year, she said that he visited the emergency department at the Riferside Medical Center several times, often staying more than four hours and in one case more than 10, before finally arriving at the behavioral care bed. Refuside refused to comment on the Rayman’s case.
During the long waiting period, Fregeau does not know what reassurance can her husband be given.
“It is difficult enough to be anyone in ER, but I cannot imagine that someone has dementia there,” she said. “When will I go?” What is happening? “
Since November, Reman has been going to MCA senior adults center in Kankakee. Freen said that REMan treats today’s position like his job, and displays emptiness and hygiene, but he returns to the house happier after spending time throughout the house and away from the house.
In Illinois, there are fewer numberAdult Day centersFrom there are provinces, and other resources for people with dementia also shrink.a reportFrom the American Health Care Association and the National Center for Living, with the help of that 1000 House for Elderly Care in the United States is closed between 2015 and 2022. At least 15 behavioral health centers, which are facilities specialized in treating mental health issues,closedIn 2023.
With fewer places for patients after exit, the hospital family is used for a longer period, which exacerbates the problem of ascension to the climb. It has become difficult to obtain a hospital specialized bed, especially when dementia causes aggression.
This was the case for a father Balhan, who became increasingly excited during his stay. Hospital staff told Han that the behavioral welfare unit was not taking dementia, so Speer was stuck in ER for 24 hours until they found a behavioral health facility separate from the health system, which would take it.
Although the hospital was unable to comment on the specific situation of Speer, a spokesperson for Heedee Health Spencer and the heir said that the behavioral care unit usually recognizes the patients of aging, including those who suffer from dementia, but this depends on factors such as bed availability and medical needs specified for the patient.
She feels that the American health care system has failed to treat her father as a human being.
She said, “It was not for me as if he was treated with any dignity as a person.” “If anything can change, that will be the change that I want to see.”
This story was originally shown on Fortune.com
https://fortune.com/img-assets/wp-content/uploads/2025/04/AP25091643610089.jpg?resize=1200,600
2025-04-15 18:56:00





